Chest High-Resolution Computed Tomography for chronic suppurative lung disease in late childhood and early adolescence: Radiation dose and image quality evaluation using iDose4 Iterative Reconstruction Algorithm
Copyright
© 2017 Upon acceptance of an article for publication in Hellenic Journal of Radiology, authors transfer copyright to the Hellenic Radiological Society but they retain the intellectual property rights including research data
Introduction
Despite the continuous new applications of Computed Tomography (CT) in everyday clinical practice, potential risks still exist from associated ionising radiation. As expected, these risks are higher for children who are under the process of growing and consequently more radiosensitive than adults [1]. In fact, recent publications have suggested associations between paediatric CT scans and malignancies such as leukaemia or brain tumours [2, 3]. Therefore, there is a great need to expose each paediatric patient to the minimal possible ionising radiation dose without affecting the diagnostic value of the CT examination.
Several radiation dose reduction techniques have been introduced so far, such as the Automatic Exposure Control (AEC) CT system and manual decrease of the acquisition settings (tube current-time product and tube voltage) according to the patient’s somatometric characteristics [4, 5]. However, the reduction of tube current-time product (mAs) or tube voltage (kVp) may be responsible for diagnostic unreliability of the CT examination because of excessive image noise. The Iterative Reconstruction (IR) algorithms of CT image reconstruction have re-emerged as an alternative radiation dose reduction technique with an advantage over the traditionally used Filtered Back Projection (FBP) reconstruction algorithm, as they satisfactory reduce image noise through a procedure of repetitive reconstructions [6]. Therefore, they provide better image quality (IQ) for the CT examination, allowing a significant radiation dose reduction for each patient [6].
So far, the number of publications concerning paediatric chest CT examinations with the use of iterative reconstruction algorithms remains limited [7, 8]. The purpose of this study is to evaluate radiation exposure reduction and IQ in High Resolution CT (HRCT) examinations for chronic suppurative lung disease in late childhood and early adolescence (children 7-13 years old, weighing >30 kgs) with the use of an IR algorithm (iDose4 Hybrid IR Algorithm, Philips Healthcare, Cleveland, OH, USA) compared to the standard FBP reconstruction algorithm. An additional purpose of the study is to determine the appropriate combination of iDose level and CT examination settings (kVp and mAs) providing acceptable CT IQ. The results of the particular study on IR algorithm use will also be compared to those of a similar study that has already been published, concerning dose reduction and image quality in children up to 10 years old with the same disease entity, but weighing less than 30 kgs [9].
Material and Methods
The present cohort study had our hospital’s ethics committee approval and was performed according to the ethical standards as described by the Declaration of Helsinki.
Patient Population
We retrospectively reviewed school-aged children and adolescents between 7 and 13 years old, who underwent chest HRCT examinations on our Radiology Department’s 64-detector row CT scanner for chronic suppurative lung disease, before and after the installation of iDose4 IR algorithm. For reasons of homogeneity, the patient sample that participated in the current study weighed ≥30 kgs. So, paediatric patients of the defined age group weighing <30 kgs had to be excluded from the study.
The retrospective review (January 2010-March 2012) showed that a total number of 13 children underwent the specific examination using the standard FBP reconstruction algorithm (“FBP protocol” group). Among those children, 11 complained of wet cough, whereas two additionally had recurrent infections of the lower respiratory tract.
After the installation of iDose4 IR algorithm in our Department, 22 paediatric patients of the same age group underwent chest HRCT examination for chronic suppurative lung disease using the IR algorithm (“iDose protocol” group) between March 2012 and January 2017. Because of poor cooperation (severe motion artefacts), four of them had to be excluded from the study. Therefore, a total number of 18 patients were included in the ‘iDose protocol’ group, 16 of which showed prolonged wet cough and two also had recurrent infections of the lower respiratory system.
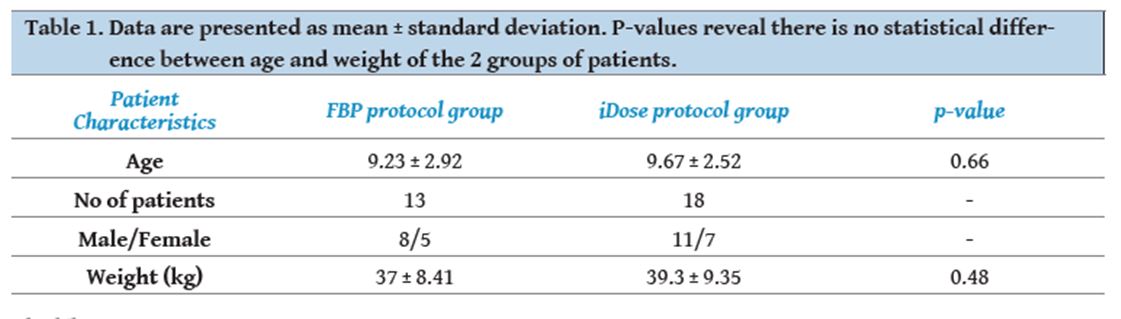
Exact weight, age and sex were recorded for all the paediatric patients of the study. No statistically significant differences were noted concerning the aforementioned parameters of the two groups of patients (Table 1).
[Figure ID: ]
Acquisition protocol
All the HRCT examinations were performed in a 64-slice multidetector CT (MDCT) scanner (Brilliance, Philips Healthcare, Cleveland, OH, USA). The “FBP protocol” group was scanned with 120 kVp and 60-120 mAs settings, whereas the “iDose protocol” group was performed with the same voltage and reduced mAs settings (20-30 mAs), using particular iDose levels (among the seven iDose levels existing, indicatively levels 2, 4 and 6 were chosen). A conservative policy concerning the tube current-time product reduction was followed based on vendor’s instructions and on measurements in a CT IQ phantom [10].
All scans in both protocols were performed without using AEC. In both groups, HRCT slices of 1.25 mm slice thickness were obtained with axial scans every 1 cm from lung apex to base for inspiratory scans, and 3-4 spaced HRCT slices were obtained for expiratory scans, using the same equipment and supine patient positioning. Protection measures were taken for the children’s genital area with lead safety clothing use (skirt lead aprons). Furthermore, for both iDose- and FBP-enabled CT image reconstructions detector configuration (64 x 0.625 mm), gantry rotation time (0.5 sec) and filter (YC) were held constant.
Radiation Exposure Quantities
Volume CT Dose Index (CTDIvol) and Dose Length Product (DLP) displayed on the CT console were used to estimate and compare radiation exposure between the two groups of patients. To obtain the effective dose (ED), DLP was multiplied by an appropriate conversion coefficient for the paediatric thorax (k=mSv·mGy−1cm−1) depending on the chosen kVp settings (120 kVp) and paediatric patient age according to ICRP Publication 103 [11]. Size-Specific Dose Estimate (SSDE) was also calculated by corrections based on the size of the paediatric patient, using the anteroposterior and lateral diameter measured on patient images at the level of the xiphoid process [12].
Subjective Image Quality
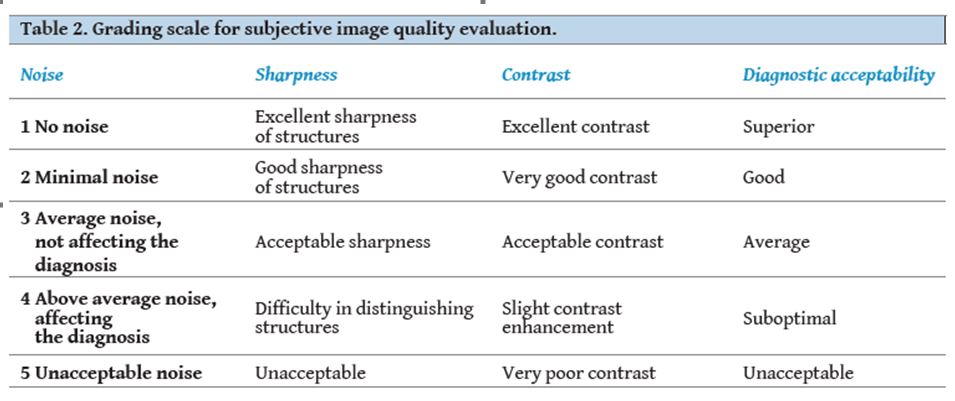
The subjective IQ score of both protocol examinations was evaluated independently by two paediatric radiologists highly experienced in paediatric chest (E.A. with 23 years of experience and A.M. with nine years of experience) for noise, sharpness, contrast and diagnostic acceptability using a descending five-point scale. According to this scale, grade 1 corresponds to excellent IQ score and grade 5 corresponds to non-acceptable IQ score, whereas grade 3 constitutes the threshold for diagnostic acceptable image (Table 2). The overall IQ score was estimated as the average value of image, sharpness and contrast scores. The presence of artefacts (respiratory, metallic, oversmoothing, blotchy or pixelated appearance etc.) affecting the diagnosis was also pointed out. Diagnostic acceptability evaluation was exclusively based on the existence of the aforementioned artefacts affecting the diagnostic outcome.
[Figure ID: ]
Objective Image Analysis
Quantitative noise measurements were conducted by locating a circular region of interest (ROI) of 40 mm2in the descending aorta and in 3 muscle groups (the paraspinal muscles, the latissimus dorsi and the infraspinous muscle), each at the level of the carina. The selected ROIs had to be homogeneous and strictly located at the same site in all paediatric patients. Objective noise was defined as the standard deviation (SD) of the attenuation values of each particular ROI.
Statistical Analysis
All data are presented as mean value ± standard deviation. Unpaired t-test was used for data statistical analysis of radiation exposure, subjective IQ score and objective image noise. Interobserver agreement between the two radiologists was evaluated using kappa (k) test with k<0.20 signified poor agreement; k=0.20-0.40 fair agreement; k=0.41-0.60 moderate agreement; k=0.61-0.80 goodagreement; and k=0.81-1.0 almost perfect agreement [13, 14]. The statistical tests were performed using the Superior Performance Software System (SPSS, v 21.0, SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered to indicate statistical significance.
Results
Radiation Exposure Quantities
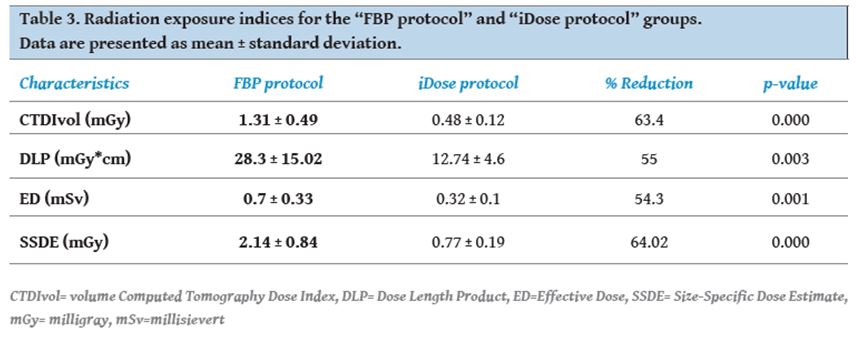
Statistical analysis revealed that the iDose4 IR algorithm use allows a significant radiation dose reduction varying from about 54% (effective dose) to 64% (SSDE), compared to the FBP algorithm (Table 3).
Subjective Image Quality
The results of subjective IQ evaluation concerning the FBP and iDose4 protocols are presented on Table 4. The interobserver agreement showed a good to almost perfect agreement between the two independently working radiologists (k>0.647) concerning both image noise and overall image quality. The overall score of the “FBP protocol” group approached excellent image (score equal to 1) and subjective image noise was evaluated as minimal (score <2).
[Figure ID: ]
Concerning the “iDose4 protocol” group, a progressive improvement in IQ score from iDose level 2 to iDose level 6 reconstruction algorithm was observed for all the aforementioned parameters (noise, sharpness, contrast and diagnostic acceptability).
It should be noted as well that all mean scores from both radiologists were from 1 to 3, even with the lowest iDose level used (iDose level 2), which is considered an acceptable score as it corresponds to satisfactory IQ without the existence of excessive noise affecting the diagnosis. Almost excellent overall IQ score, comparable to the “FBP protocol” group overall IQ score, was obtained with iDose level 6 (p=0.659). It should also be pointed out that noise was comparable between the two groups of patients with iDose level 4 (p=0.743) and there also seemed to be a reduction of noise using iDose level 6, but not a statistically significant one (p=0.106) (Table 4).
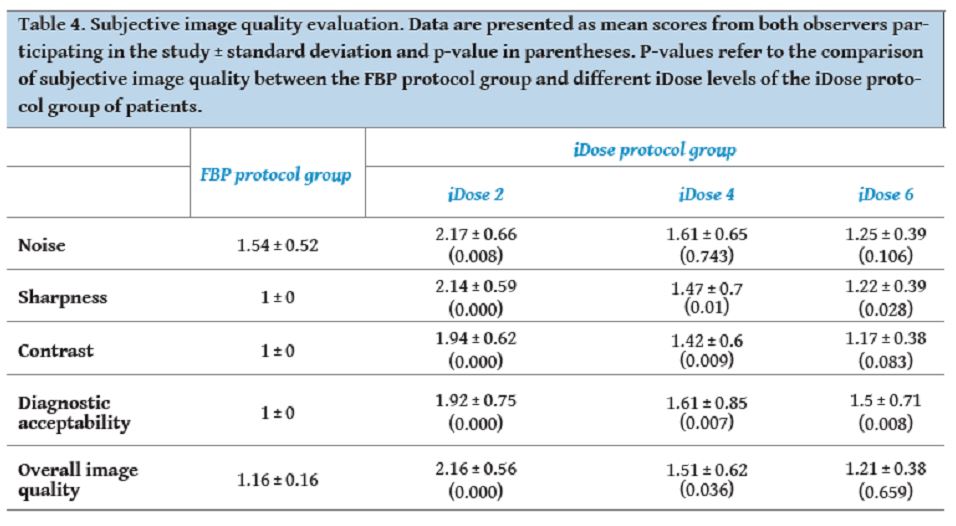
[Figure ID: ]
There was also an assessment of the presence of artefacts affecting the diagnosis, such as respiration artefacts and in one case artefacts from metallic implants due to bone fracture restoration. The existence of these artefacts in most of the cases affected the diagnostic acceptability, but not so much as to render the examinations non-diagnostic (scores up to 3). Additionally, artefacts responsible for blotchy or pixelated appearance already described in literature [7, 8] were not observed in this study. Oversmoothing artefacts coming from the use of high levels of IR algorithms also described in literature were only noticed in a small number of children with iDose level 6 (4/18 children), but still they didn’t affect significantly the diagnostic outcome, as diagnostic acceptability wasnever evaluated with score >2 from neither of the radiologists participating in the study.
Objective Image Quality
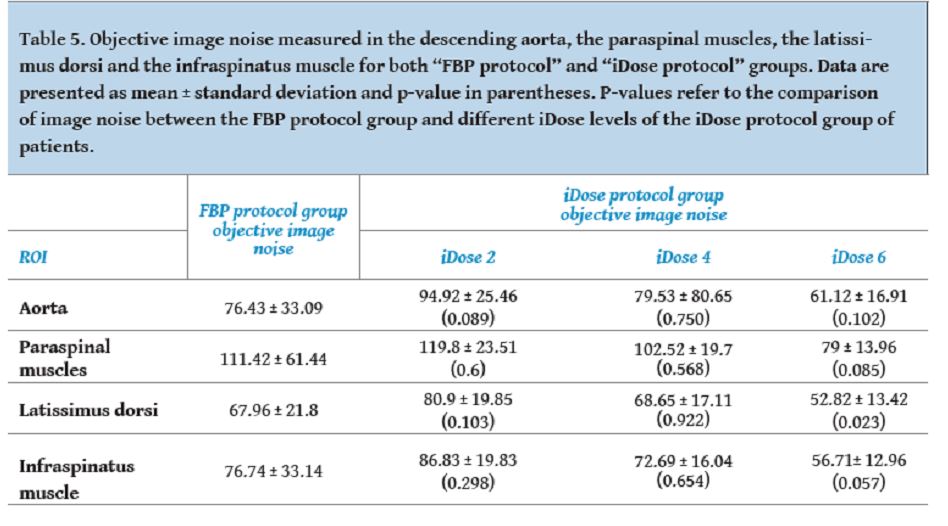
Objective IQ assessment in the ‘iDose4 protocol’ group showed a gradual reduction of noise from iDose level 2 to progressively higher levels of iDose (Table 5).
Image noise with the “iDose4 protocol” group was comparable with the “FBP protocol” group noise by using iDose level 2 (p>0.005 at all ROIs), whereas there seemed to be statistically significant noise reduction (latisssimus dorsi, p=0.023) with the use of the highest iDose level used in this study (iDose level 6) (Table 5).
Among the four ROIs, better results were noticed in the infraspinatus and latissimus dorsi muscles and worse in descending aorta and paraspinal muscles, possibly having to do with beam hardening artefacts induced by adjacent bones (costae and vertebrae).
[Figure ID: ]
Discussion
Chronic suppurative lung disease (CSLD), most frequently presenting in preschool age, is attributed to recurrent viral respiratory infections [15]. It is characterised by excessively prolonged wet cough without findings of bronchiectasis from chest HRCT examination [16] and it is also associated with pathological conditions, such as cystic fibrosis, congenital malformations, primary ciliary dyskinesia syndrome (PCDS) etc. (Fig. 1). Its early diagnosis and treatment with antibiotics is of great importance as it may prevent permanent bronchi dilatation in children [16, 17].
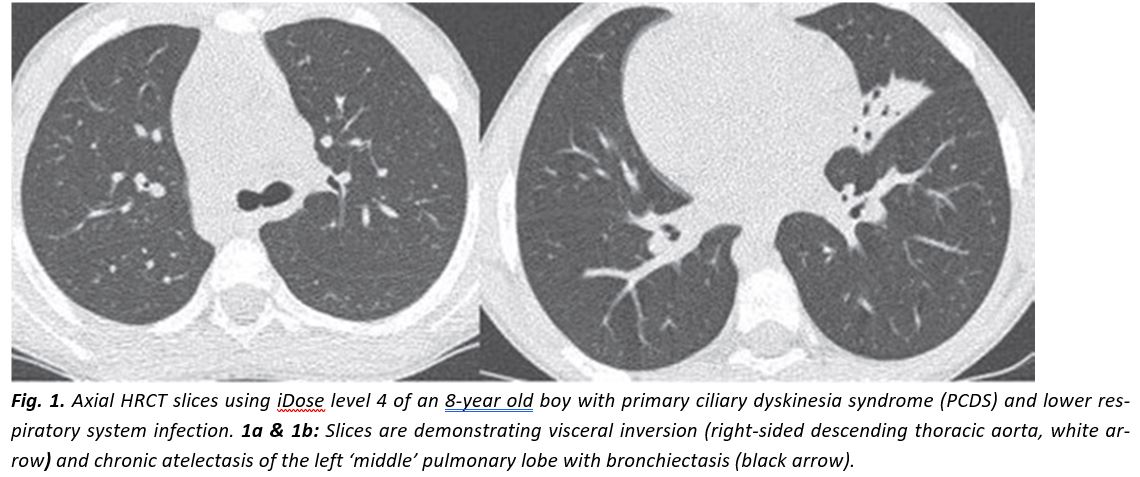
[Figure ID: ]
Imaging examinations for the investigation of CSLD are bronchoscopy, plain radiography and chest HRCT. Although bronchoscopy is the gold standard method for revealing structural airway abnormalities, it is invasive and produces temporary deterioration of respiratory function. In addition, it is not easily acceptable by children and therefore it usually requires general anaesthesia. On the other hand, plain radiography is non-invasive with low radiation exposure, but it is insensitive for diagnosing bronchiectasis. Chest HRCT on the contrary is the imaging examination required to confirm the existence of irreversible airway dilatation, as well as the severity and extent of the disease (Fig. 2).
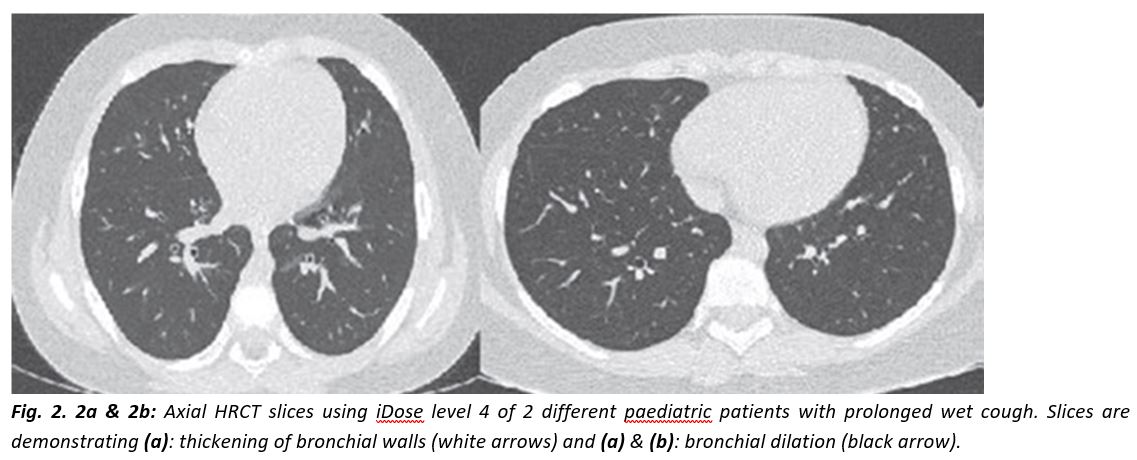
[Figure ID: ]
Nevertheless, concern still exists towards HRCT use because of the inevitably higher radiation exposure compared to plain radiography, especially in children who are more radiosensitive than adults [15, 17]. Application however of the already mentioned hybrid IR algorithms in children with CSLD could turn chest HRCT into the low-dose gold standard method for the diagnosis of bronchiectasis.
Hybrid IR anoise, while they maintain the details of anatomic CT structures (Fig. 3) [6]. Results from studies in phantoms and adults with the above IR techniques have shown significant dose reduction while maintaining, or even in some cases enhancing, IQ at lower exposure settings [18, 19]. Similar results derive as well from studies in phantoms and paediatric population. More specifically, according to Brady et al. a 40% ASIR usage allows a 42% to 48% dose reduction at all paediatric ages without seriously affecting image quality or image noise [20], whereas according to Greffier et al., the use of AEC/IR in phantoms preserves image quality with lower dose delivered [21].
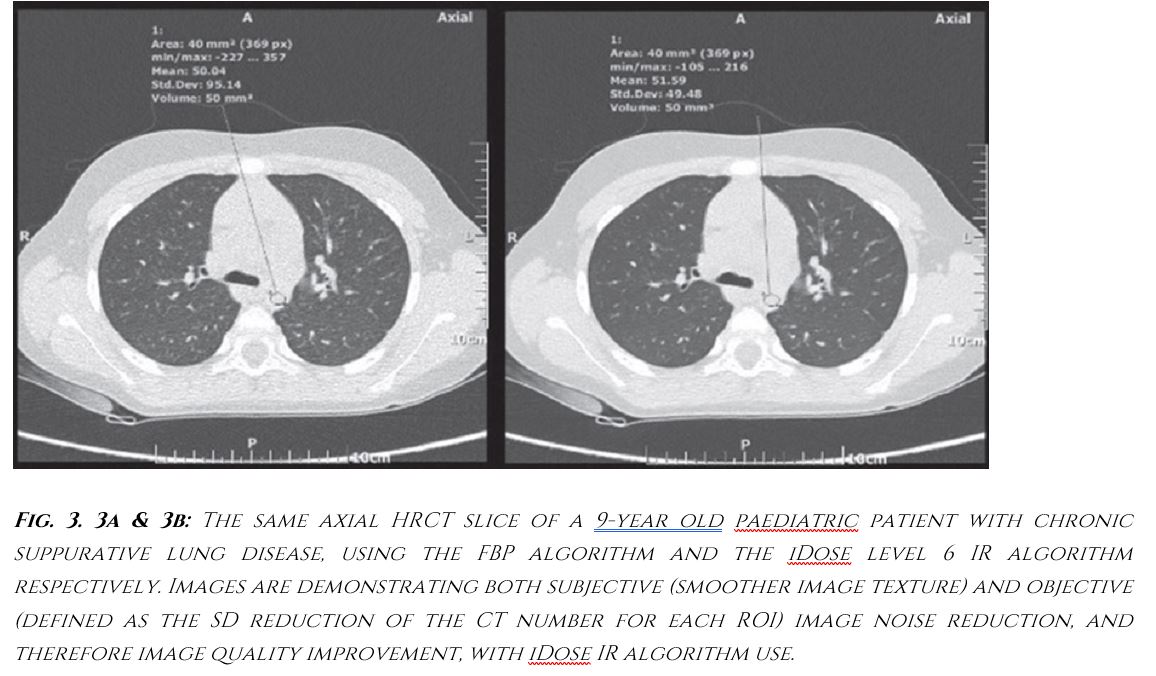
[Figure ID: ]
Nowadays, more advanced reconstruction algorithms called “model-based IR algorithms” have been developed, which approximate even more true iterative reconstruction compared to the aforementioned hybrid iterative algorithms. As expected, these algorithms significantly reduce image noise and induce even greater dose reduction, up to 92% [22]. However, further research about paediatric use of these very recently introduced algorithms has to be made, as not much information is available in the existing literature [22-25].
The already mentioned hybrid iDose4 IR algorithm, which has been installed at our Department’s 64-detectorrow CT scanner, allows reconstruction levels (from 1 to 7) to be selected before the scan or after the acquisition of raw data [26]. In order to retain comparable noise and IQ with FBP algorithm use, the appropriate iDose level should be selected according to the chosen percentage of dose reduction [27] and in order to increase image resolution, higher iDose levels should be applied [26].
Despite the aforementioned advantages of IR algorithm use, the number of publications concerning IR application in children’s chest remains limited so far. To our knowledge, this is the second study concerning iDose4 IR application exclusively in paediatric chest CT, with the first one focusing on pre-school aged children undergoing chest HRCT for the same clinical indication. A small number of recent studies in paediatric chest CT with the use of a low-dose protocol with 30% (Singh et al., 2012) and 50% ASIR (Lee et al., 2012) have demonstrated a 46.4% and a 55.2% reduction in effective dose respectively [7, 8]. In the current study, the effective dose reduction with the use of iDose4 IR algorithm is 54.3%, with SSDE reduction being 64%. That is to say results comparable to the aforementioned studies.
The observed lower degree of dose reduction in the current study focused on children heavier than 30 kg compared to a previous study on children weighing <30 kg in which SSDE dose reduction exceeded 80% [9] is mainly attributed to our conservative policy towards mAs diminution in this age group of patients. More specifically, as quite low mAs settings were already used in these children before the installation of the iDose4 IR algorithm, a more aggressive reduction when setting the examination protocol after the installation of the IR algorithm was considered quite risky for the diagnostic outcome of the CT examinations. However, subjective image quality evaluation of the current study revealed that the diagnostic outcome after IR algorithm use was more than satisfactory and further dose reduction with even lower mAs settings could be achieved, without seriously affecting the diagnostic reliability. From a clinical point of view, this conclusion is of great importance for children suffering from CSLD, as these children are in need of repetitive radiological examinations in order to get proper diagnosis and treatment. Therefore, high quality CT examinations and the lowest possible radiation exposure are both necessary for these patients.
As already mentioned, the aim of this study, apart from proving significant radiation dose reduction with the use of iDose4 IR algorithm, was also to determine the appropriate combination of iDose level and CT examination settings (kVp and mAs), providing acceptable CT IQ. Studies for chest CT with a similar reasoning that have been conducted so far are: a) one for adults by Singh et al., using 30%, 50%, and 70% of ASIR blending [28], where mild pixilated blotchy texture was noticed with 70% blended ASIR images and b) one by B. Karmzyn et al. for children with FBP and iDose levels 2 to 6, according to which iDose level 3 or 4 was optimal for most cases [29]. According to our study, iDose level 4 could be safely used with our chosen kVp and mAs settings, since no blotchy, pixilated or oversmoothing artefacts were noticed and subjective IQ results were comparable to those of the FBP group of patients with this iDose level. Concerning iDose level 6 use, despite the fact that overall IQ score was comparable to the IQ score of the FBP group of patients, oversmoothing artefacts were noticed in a small number of patients (four children) causing diagnostic insecurity to the radiologists participating in the study. More specifically, the existence of these artefacts provided a final image outcome, not familiar to our radiologists raising issues of diagnostic reliability, despite the fact that comparison with lower iDose levels showed no major diagnostic information loss.
An additional important observation of the particular study was that subjective overall IQ score was always evaluated up to 3, meaning that all CT images were considered to be diagnostically acceptable, even those with the lowest iDose level used (iDose level 2). Comparable results of subjective and objective evaluation between the two groups of patients (“FBP protocol” and “iDose4 protocol” group) in the current study existed with lower iDose level use compared to a previously published study on pre-school aged children also with CSLD. Specifically, comparable subjective image noise between the two groups of patients was obtained with the use of iDose level 4 instead of iDose level 6 of the previous study and comparable objective image noise was achieved with the lowest iDose level used in this study (iDose level 2), in contrast to iDose level 6 of the aforementioned study [9]. All the above results indicate that further dose reduction could be achieved with the use of even lower mAs settings (lower than 20 mAs) in the current study despite our initial diffidences, without actually affecting the diagnostic outcome.
Among the limitations of this particular study concerning chest HRCT for chronic suppurative lung disease was the small number of the participating paediatric patients. This is mainly attributed to the, so far limited, use of HRCT in these cases because of concern towards young patients’ radiation exposure, and to the lower incidence of the disease in late childhood as already explained [16]. The limited number of patients participating in the study can be attributed to the fact that, despite the older age, there still was a small number of non-cooperative patients during the CT scans (4 children), that had to be excluded from the study due to significant motion artefacts affecting the diagnosis.
Another limitation of the study was the fact that all the HRCT examinations were conducted without using the AEC system. However, AEC application was not considered necessary for the current study, as already low mAs settings were used even for the FBP protocol group of patients (low-dose CT protocol). With AEC application as well, off-center positioning of non-cooperative children would result in excessive reduction in tube current and very noisy images affecting the diagnostic outcome [30].
A final limitation of the current study was the fact that we only focused on quantitative and qualitative criteria for image quality evaluation, without evaluating relevant criteria for diagnostic quality evaluation (investigation of imaging findings specific to the particular disease entity). This approach however could be considered for future studies.
In conclusion, the current study proved significant radiation dose reduction with the iDose4 application in paediatric patients weighing >30 kg undergoing chest HRCT for chronic suppurative lung disease, without deterioration of CT image quality. A combination of iDose level 4 with our study’s examination settings (kVp, mAs) is recommended, as it provides comparable IQ scores with FBP algorithm use, without the existence of oversmoothing artefacts affecting the diagnosis. A wider use of IR algorithms could be established in the future in paediatric chest HRCT, especially for those children in need for repetitive radiological examinations.References
1.Ogbole GI. Radiation dose in pediatric computed tomography: risks and benefits.Ann Ib Postgrad Med2010; 8(2): 118-126.
2.Mathews JD, Forsythe AV, Brady Z, et al. Cancer risk in 680 000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians.BMJ2013; 346: f2360.
3.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study.Lancet2012; 380(9840): 499-505.
4.Kalra MK, Maher MM, Toth TL, et al. Techniques and applications of automatic tube current modulation for CT.Radiology2004; 233(3): 649-657.
5.Kalra MK, Maher MM, Toth TL, et al. Strategies for CT radiation dose optimization.Radiology2004; 230(3): 619-628.
6.Hara AK, Paden RG, Silva AC, et al. Iterative reconstruction technique for reducing body radiation dose at CT: feasibility study.AJR Am J Roentgenol2009; 193(3): 764-771.
7.Singh S, Karla MK, Shenoy-Bhangle AS, et al. Radiation dose reduction with hybrid iterative reconstruction for pediatric CT.Radiology2012; 263(2): 537-546.
8.Lee SH, Kim MJ, Yoon CS, Lee MJ. Radiation dose reduction with the adaptive statistical iterative reconstruction (ASIR) technique for chest CT in children: An intra-individual comparison.Eur J Radiol2012; 81(9): e938-943.
9.Smarda M, Efstathopoulos E, Mazioti A, et al. High-resolution computed tomography examinations for chronic suppurative lung disease in early childhood: radiation exposure and image quality evaluations with iterative reconstruction algorithm use.Can Assoc Radiol J2016; 67(3): 218-224.
10.Kordolaimi S, Saradeas I, Ploussi A, et al. Introduction of an effective methodology for the optimization of CT protocols using iterative reconstruction algorithms: Comparison with patient data.AJR Am J Roentgenol2014; 203(4): W434-439.
11.The 2007 Recommendations of the International Commission on Radiological Protection.ICRP Publication 103.Ann ICRP 2007; 37(2-4): 1-332.
12.Boone J, Strauss K, Cody D, et al. Size specific dose estimates (SSDE) in pediatric and adult body CT examinations. Report of AAPM Task Group 204. College Park: American Association of Physicists in Medicine, 2011.
13.Mary L. McHugh. Interrater reliability: the kappa statistic.Biochem Med(Zagreb) 2012; 22(3): 276-282.
14.Shweta, Bajpai RC, Chaturvedi HK. Evaluation of inter-rater reliability for observational data: an overview of concepts and methods.J Indian Acad Appl Psychol2015; 41(3): 20-27.
15.Couriel J. Assessment of the child with recurrent chest infections.Br Med Bull2002; 61: 115-132.
16.Chang AB, Grimwood K, Maguire G, et al. Management of bronchiectasis and chronic suppurative lung disease in Indigenous children and adults from rural and remote Australian communities.Med J Aust2008; 189(7): 386-393.
17.Nikolaizik WH, Warner JO. Aetiology of chronic suppurative lung disease.Arch Dis Child1994; 70(2): 141-142.
18.Prakash P, Kalra MK, Ackman JB, et al. Diffuse lung disease: CT of the chest with adaptive statistical iterative reconstruction technique.Radiology2010; 256(1): 261-269.
19.Prakash P, Kalra MK, Digumarthy SR, et al. Radiation dose reduction with chest computed tomography using adaptive statistical iterative reconstruction technique: initial experience.J Comput Assist Tomogr2010; 34(1): 40-45.
20.Brady SL, Yee BS, Kaufman RA. Characterization of adaptive statistical iterative reconstruction algorithm for dose reduction in CT: a pediatric oncology perspective.Med Phys2012; 39(9): 5520-5531.
21.Greffier J, Pereira F, Macri F, et al. CT dose reduction using automatic exposure control and iterative reconstruction: a chest paediatric phantoms study.Phys Med2016; 32(4): 582-589.
22.Miéville FA, Berteloot L, Grandjean A, et al. Model-based iterative reconstruction in pediatric chest CT: assessment of image quality in a prospective study of children with cystic fibrosis.Pediatr Radiol2013; 43(5): 558-567.
23.Villanueva-Meyer JE, Naeger DM, Courtier JL, et al. Pediatric chest CT at chest radiograph doses: when is the ultralow-dose chest CT clinically appropriate?Emerg Radiol2017; 24(4): 369-376.
24.Sun J, Zhang Q, Hu D, et al. Improving pulmonary vessel image quality with a full model-based iterative reconstruction algorithm in 80kVp low-dose chest CT for pediatric patients aged 0-6 years.Acta Radiol2015; 56(6): 761-768.
25.Kim HJ, Yoo SY, Jeon TY, et al. Model-based iterative reconstruction in ultra-low-dose pediatric chest CT: comparison with adaptive statistical iterative reconstruction.Clin Imaging2016; 40(5): 1018-1022.
26.Geyer LL, Schoepf UJ, Meinel FG, et al. State of the art: iterative CT reconstruction techniques.Radiology2015; 276(2): 339-357.
27.Laqmani A, Buhk JH, Henes FO, et al. Impact of a 4th generation iterative reconstruction technique on image quality in low-dose computed tomography of the chest in immunocompromised patients.Rofo2013; 185(8): 749-757.
28.Singh S, Kalra MK, Gilman MD, et al. Adaptive statistical iterative reconstruction technique for radiation dose reduction in chest CT: a pilot study.Radiology2011; 259: 565-573.
29.Karmazyn B, Liang Y, Ai H, et al. Optimization of hybrid iterative reconstruction level in pediatric body CT.AJR Am J Roentgenol2014; 202(2): 426-431.
30.Karla MK, Maher MM, Toth TL et al. Techniques and applications of automatic tube current modulation for CT.Radiology2004; 233(3): 649-654.
Ready - Made Citation
Smarda M, Efstathopoulos E, Ploussi A, Mazioti A, Kordolaimi S, Kelekis NL, Alexopoulou E. Chest High-Resolution Computed Tomography for chronic suppurative lung disease in late childhood and early adolescence: Radiation dose and image quality evaluation using iDose4 Iterative Reconstruction Algorithm.Hell J Radiol2018; 3(2): 21-31.
None
Refbacks
- There are currently no refbacks.







