Painful shoulder
Copyright
© 2016 Upon acceptance of an article for publication in Hellenic Journal of Radiology, authors transfer copyright to the Hellenic Radiological Society but they retain the intellectual property rights including research data
Part a
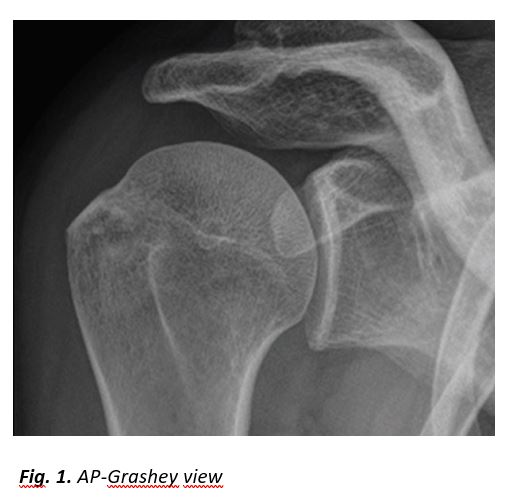
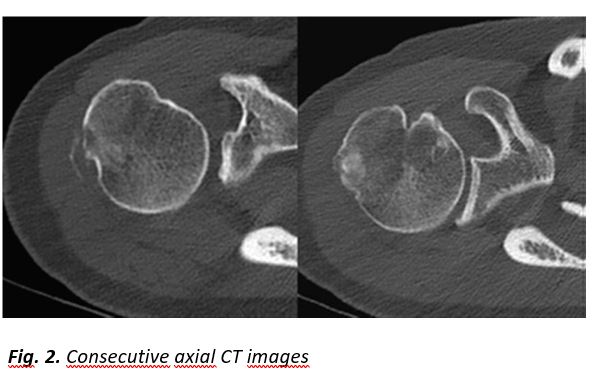
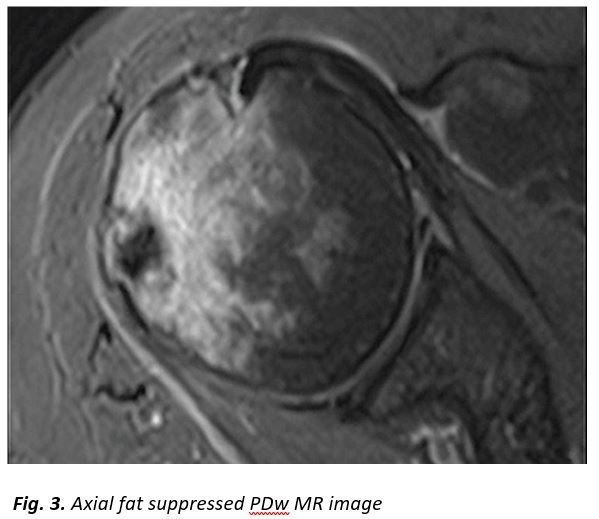
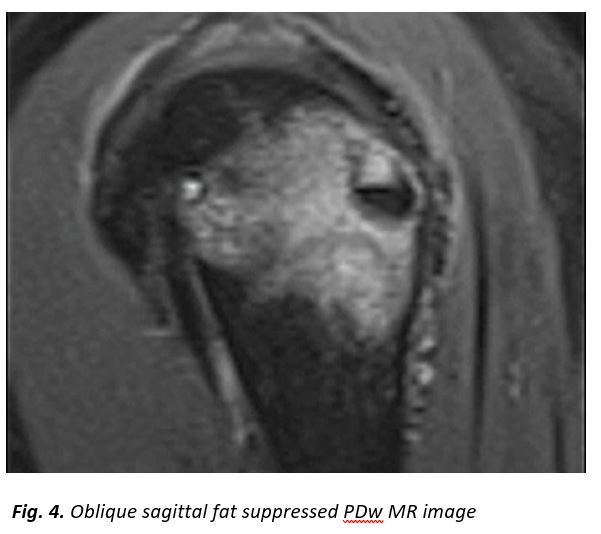
A 52-year-old female patient presented with a history of two-month right shoulder pain, more intense at night. Clinical examination showed a painful joint with limited range of motion. The painful syndrome did not respond to non-steroidal anti-inflammatory drugs (NSAIDs), analgesics and physiotherapy.Plain radiograph, CT and MR imaging are shown.
[Figure ID: ]
[Figure ID: ]
[Figure ID: ]
[Figure ID: ]
Part b
Diagnosis: Intraosseous HADD
Rotator cuff hydroxyapatite deposition disease (HADD), also known as calcific tendinopathy, calcific periarthritis or basic calcium phosphate crystal deposition disease, is a common disorder with a reported incidence of up to 22% [1]. Supraspinatus represents the most common location of HADD followed by infraspinatus, teres minor, and subscapularis [2]. Other locations include the tendons around the knee and hip joints. One of the complications of HADD is migration of the calcifications to adjacent bone through the disrupted cortex at the insertion site of the initially affected tendon. An osteolytic lesion may coexist with the intraosseous calcifications. This rare complication is known as intraosseous HADD. Osseous involvement in HADD was first reported by Hayes et al. [3] with cortical erosions at the pectoralis major, gluteus maximus, and adductor magnus tendinous insertions. Till today, several case reports and few larger series have described the osseous involvement at different sites. Although the pathogenesis of bone erosion remains unclear, it is believed that active inflammation and local vascularization at tendon insertion or mechanical effects of muscle traction may play a role in the development of cortical erosions [4]. This complication can be mistaken as an osseous tumour or infection and thus familiarity with the imaging features is important [5,6].
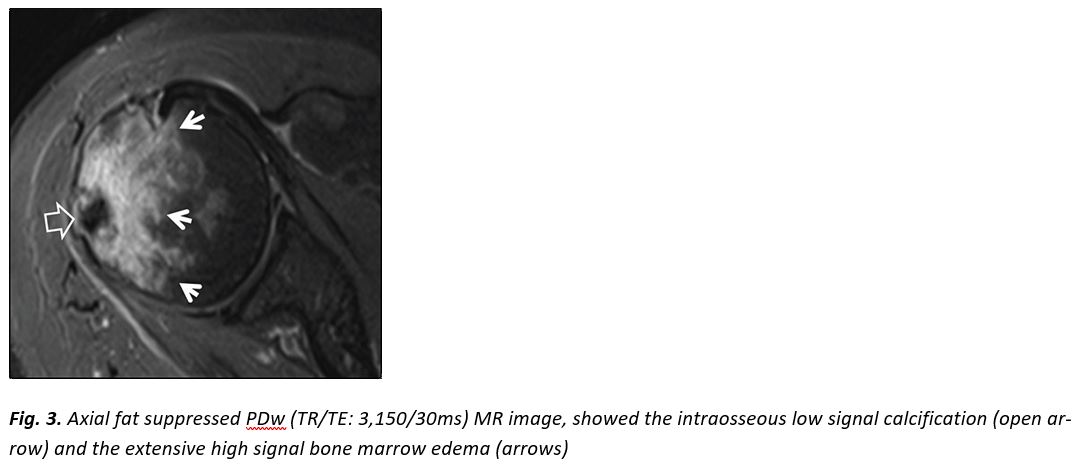
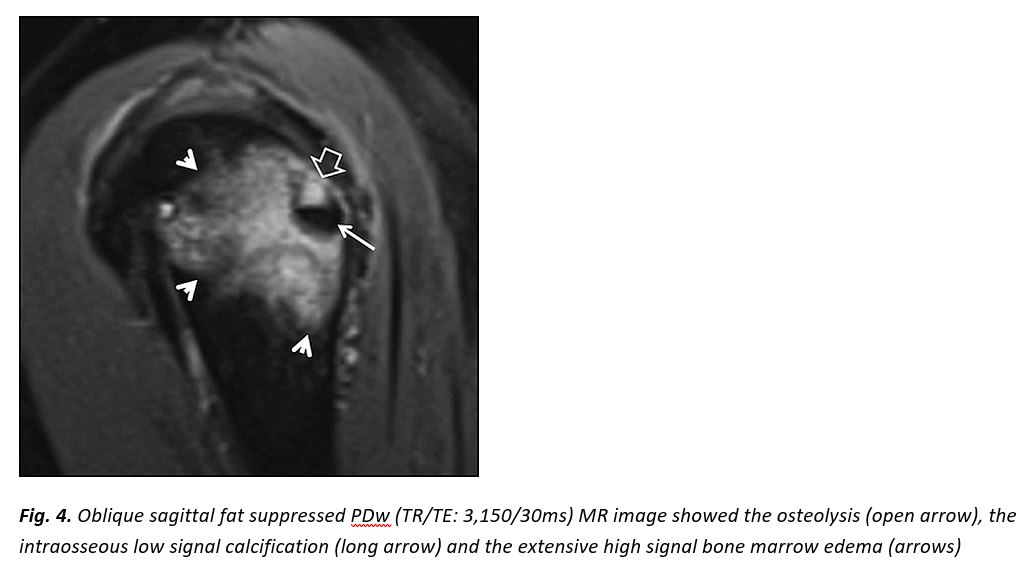
Plain X-rays and ultrasound (US) are the first line imaging modalities which can assist the diagnosis of HADD, as they can reveal the calcifications within or adjacent to the tendons. On MR imaging, tendinous and peritendinous calcific deposits appear as low or mixed low and intermediate signal intensity lesions on both T1w and fat suppressed PDw MR images, with surrounded soft-tissue edema. Gradient echo sequences show the calcifications to better advantage. The signal intensity at the site of the cortical erosion is low on T1w and heterogeneous on fat-suppressed PD/T2w sequences [7]. Intraosseous calcium deposits may be of very low signal intensity on both T1w and fluid sensitive MR images, or show heterogeneous T2 appearance, depending on the stage of the disease. Varying degree of surrounding BME is usually present. No major reports exist on the evaluation of intraosseous HADD with US.
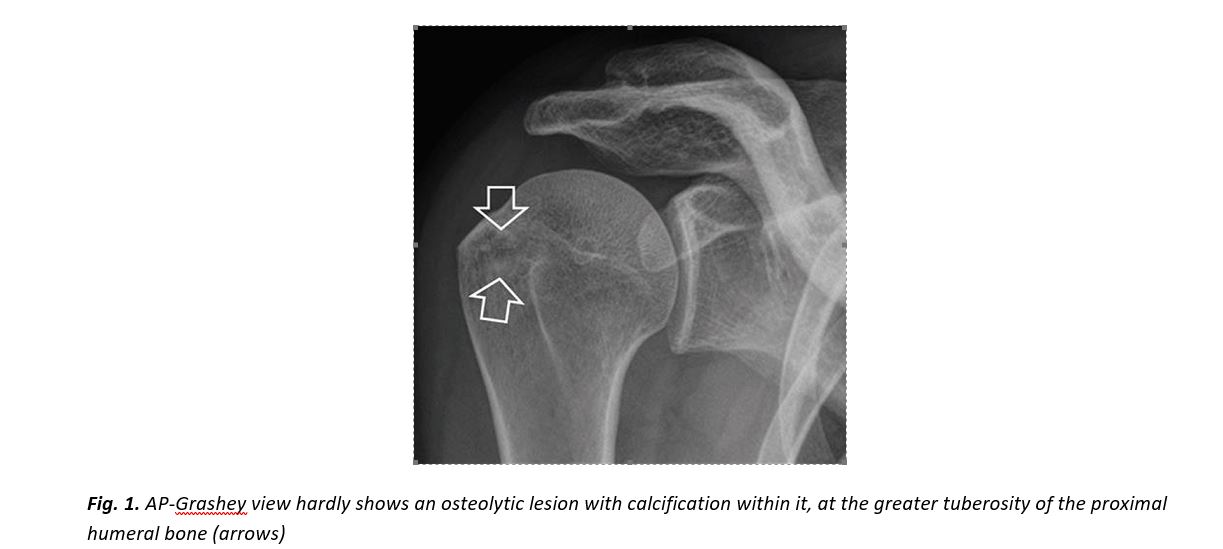
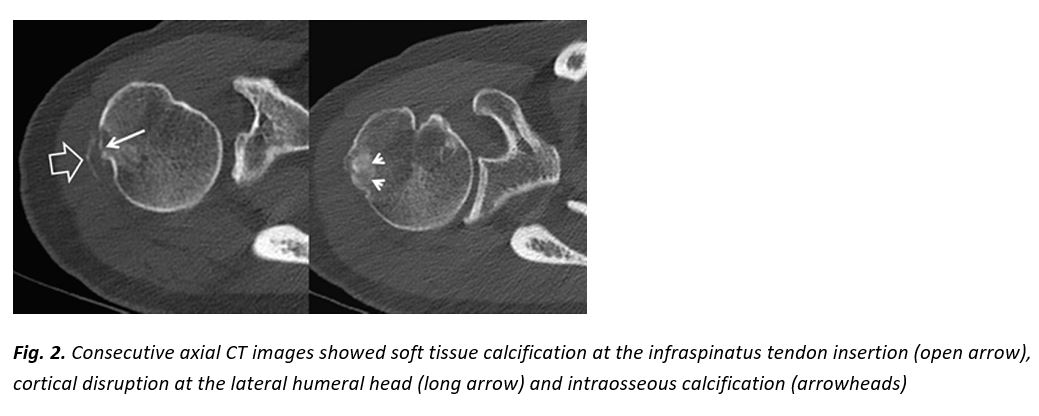
In our patient, radiologic investigation included plain films, CT and MR imaging of the right shoulder. Imaging showed parosteal calcification at the level of the infraspinatus insertion, cortical disruption at the lateral humeral head, an osteolytic lesion with calcification within it and extensive surrounding bone marrow edema (Fig. 1-4).
NSAIDs combined with physiotherapy are the mainstay of nonoperative treatment for shoulder HADD [8]. Arthroscopic treatment is less effective than in classic location within or adjacent to a tendon [10]. Thus arthroscopy is considered nowadays as the last option only when other methods have failed [9]. According to our experience (unpublished data on 4 patients), a combined approach with US guided barbotage for the soft tissue and CT guided aspiration for the intraosseous calcifications, is efficient in patients with persistent symptoms. HADD is self limited and our patient showed moderate improvement at the 6-month clinical follow-up following physiotherapy.
[Figure ID: ]
[Figure ID: ]
[Figure ID: ]
[Figure ID: ]
Conflict of interest:
The authors declared no conflicts of interest.
Corresponding Author, Guarantor
Apostolos Karantanas, Professor of Radiology, University of Crete, Stavrakia, 71110, Heraklion, Crete, Greece, E-mail: akarantanas@gmail.com
References
1.Oliva F, Via AG, Maffulli N. Calcific tendinopathy of the rotator cuff tendons.Sport Med Arthrosc Rev2011; 19(3): 237-243.
2.Sussmann AR, Cohen J, Nomikos GC, et al. Magnetic resonance imaging of shoulder arthropathies.Magn Reson Imaging Clin N Am2012; 20(2): 349-371.
3.Hayes CW, Rosenthal DI, Plata MJ, et al. Calcific tendinitis in unusual sites associated with cortical bone erosion.AJR Am J Roentgenol1987; 149(5): 967-970.
4.Durr HR, Lienemann A, Silbernagi H, et al. Acute calcific tendinitis of the pectoralis major insertion associated with cortical bone erosion.Eur Radiol1997; 7: 1215-1217.
5.Porcellini G, Paladini P, Campi F, et al. Osteolytic lesion of greater tuberosity in calcific tendinitis of the shoulder.J Shoulder Elb Surg2009; 18(2): 210-215.
6.Martin S, Rapariz JM. Intraosseous calcium migration in calcifying tendinitis: A rare cause of single sclerotic injury in the humeral head.Eur Radiol2010; 1284-1286.
7.Flemming DJ, Murphey MD, Shekitka KM, et al. Osseous involvement in calcific tendinitis: A retrospective review of 50 cases.AJR Am J Roentgenol2003; 181(4): 965-972.
8.Lanza E, Banfi G, Serafini G, et al. Ultrasound-guided percutaneous irrigation in rotator cuff calcific tendinopathy: What is the evidence? A systematic review with proposals for future reporting.Eur Radiol2015; 25: 2176-2183.
9.Seyahi A, Demirhan M. Arthroscopic removal of intraosseous and intratendinous deposits in calcifying tendinitis of the rotator cuff.Arthroscopy2009; 25(6): 590-596.
10.Porcellini G, Paladini P, Campi F, et al. Arthroscopic treatment of calcifying tendinitis of the shoulder: Clinical and ultrasonographic follow-up findings at two to five years.J Shoulder Elb Surg2004; 33(10): 596-599.
Ready - Made Citation
Mandrillo D, Psaras K, Karantanas A. Painful shoulder.Hell J Radiol2016; 1(1): 78-81.
None
Refbacks
- There are currently no refbacks.







